PCOS Case Study: Best Practices for LH Testing and BBT Tracking
I personally learn best when I’m able to see real-life case studies. In the spirit of deepening shared knowledge on fertility charting, especially in longer cycles, I wanted to share a deep dive into my experience tracking multiple cycle biomarkers in a PCOS cycle.
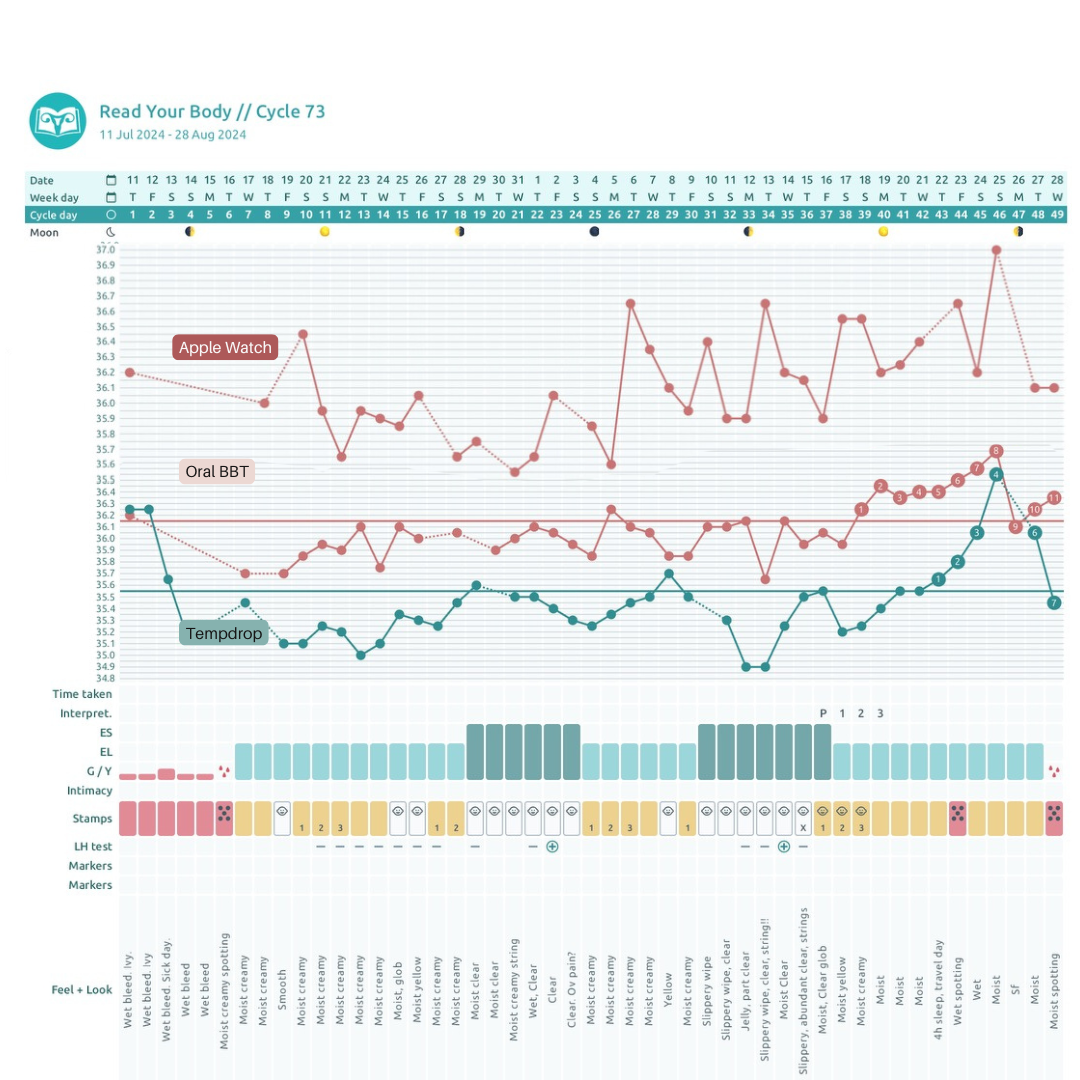
In this post I’ll share my journey of testing out two different types of LH tests (quantitative and qualitative) and three basal body temperature devices (Apple Watch, Oral BBT, and Tempdrop) to see how they performed.
Let’s dive into this detailed case study where we compare different LH tests and temperature devices to find the most accurate tools for tracking a PCOS cycle. Discover the strengths and weaknesses of each method and learn valuable tips for your fertility awareness journey with PCOS.
Yes, I’ve had long cycles for a long time. Read more about charting with irregular cycles here.
Understanding PCOS and Its Impact on Cycle Tracking
Before we jump into the nitty-gritty, let’s chat about PCOS and why it makes cycle tracking a unique adventure. PCOS is a hormonal disorder that can cause irregular menstrual cycles, longer cycles, and sometimes no ovulation at all. This can make fertility charting a little tricky. But, as you can see from my fertility chart, knowing when you ovulate with PCOS can bring peace of mind to a longer cycle.
The Case Study: My PCOS Cycle
Let’s set the stage: my cycle spanned from July 11, 2024, to August 28, 2024, making it a longer one—typical of PCOS. With this cycle, I wanted to put a few different tools to the test to see how they would handle the ups and downs of an unpredictable cycle like this one. Spoiler alert: not all tools are created equal!
Testing Different LH Tests: Quantitative vs. Qualitative
First up, LH tests! Tracking the surge in LH before ovulation is what we’re on the lookout for when trying to confirm ovulation. But here’s the kicker: with PCOS, things are a little more complex. In short, I would not recommend relying solely on LH tests to identify your fertile window, especially with PCOS.
This is because another key feature of PCOS is imbalanced ratios of LH. High insulin levels cause the pituitary gland to release more LH, resulting in an imbalanced ratio of LH to FSH (often 2:1 or 3:1). This imbalance means ovarian cells can't convert androgens to estrogen effectively. As a result, estrogen levels drop, and androgen levels rise. High androgen levels interfere with normal follicle development, leading to the formation of multiple small cysts on the ovaries, characteristic of PCOS.
The challenge with LH testing and PCOS is twofold. First, a long follicular phase, and not knowing when ovulation happens ahead of time, means that you may use many LH tests before you get a positive. Second, baseline elevated levels of LH may mean that it’s more common that you’ll get a false positive.
Quantitative LH Tests: The Numbers Game
Quantitative LH tests measure the exact concentration of LH in your urine, giving you a detailed readout of your hormone levels. I know, sounds fancy, right? And honestly, they kind of are! These tests were fascinating for me in this cycle because they showed me exactly what was going on, day by day. They can be easily read by comparing the test line to the test reading tool included in the box, or by using the Premom app.
The Good: Easier to read than threshold tests in PCOS cycles where LH may be elevated.
The Not-So-Good: The Premom app isn’t foolproof. The app misidentified an LH surge by looking at patterns in the LH tests, rather than the individual tests. Had I not been charting mucus and temperature, I would have inaccurately interpreted my chart.
Qualitative LH Tests: The Quick and Easy Option
Now, qualitative LH tests are like the laid-back siblings of the quantitative tests. They give you a straightforward yes or no answer: "Are you surging? Yes or no?" Easy peasy. These are great for a quick check but come with their own set of challenges in a PCOS cycle.
The Good: Super simple to use and easy on the wallet. Suitable for most charters. No need to decipher numbers; just look for a positive or negative result.
The Not-So-Good: They might miss those subtle rises in LH, and in theory, they may result in more false positives.
In This Cycle: I used the Premom app to interpret results for both tests, and I saw just how wrong the app can be. Because it looks for patterns as well as positive/negative test results, when I had a slight surge of LH that wasn’t quite ovulation (typical of PCOS), it marked it as LH positive or peak. However, I never confirmed ovulation with my other biomarkers.
When I finally did ovulate, I was able to recognize a clear positive with my own eyes in both types of tests. A good reminder to take any type of algorithm in an app with a grain of salt!
Temperature Devices: The Showdown
Now, let’s talk temperatures! Charting basal body temperature (BBT) is another key piece of the fertility awareness puzzle. For this cycle, I tested out three different temperature devices: the Apple Watch, a traditional Oral BBT thermometer, and the Tempdrop sensor. Here’s how they stacked up:
Apple Watch: A Swing and a Miss
I was curious to see my temps with Apple Watch, but let’s just say it didn’t quite make the grade. While it’s been interesting to track everything else with my Apple Watch (sleep and exercise), the temperature data was all over the place: no clear pattern, just a lot of ups and downs.
The Verdict: Not reliable for BBT tracking, especially in a PCOS cycle where consistency is key.
Oral BBT Thermometer: The Gold Standard
The Oral BBT thermometer, my tried and true method, came through like a champ. It gave me the clearest, most consistent data, which is exactly what I needed to track ovulation.
The Verdict: Reliable and accurate. If you’re willing to commit to the daily routine, this one’s a winner.
Tempdrop Sensor: The Middle Ground
The Tempdrop sensor offered a middle-of-the-road option. It was more precise than the Apple Watch, but I experienced a delayed shift this cycle.
The Verdict: Tempdrop is a decent alternative if you’re looking to sleep in and get accurate readings, but you may want to cross check with an oral thermometer and ensure you’ve got accurate placement, as placement can make a huge difference in the accuracy of temps.
I’m tracking Billings categories and FEMM categories with mucus this cycle. While I had hormonal changes that resulted in changes to my cervical mucus, the most distinct change was when I actually was able to confirm ovulation. My mucus followed a very particular pattern (called “Peak”) when I finally did ovulate.
Your mucus can change and not necessarily end in ovulation. However, you’ll likely experience a very specific pattern in your cervical mucus when you do eventually ovulate, along with confirming ovulation with your other ovulation crosschecks, such as BBT.
And if you wanna learn more about your CM, you’ll want to read my Ultimate Guide to Cervical Mucus with Photos, here.
Unique Circumstances This Cycle
Okay, so let’s get into why this particular cycle was so special (aside from the obvious PCOS factor). I had a lot going on: stress levels were higher than usual, and I was traveling, which threw off my routine a bit. All these factors could have impacted my hormone levels and my body’s temperature regulation. It’s a good reminder to keep track of any disturbance in your chart, including travel and anything out of the ordinary.
Interpreting the Data: Lessons Learned
Here’s the takeaway: when you’re dealing with a PCOS cycle, not all fertility awareness tools are going to work perfectly. Sometimes you need to experiment to find what is going to be the most accessible and most consistent for you. If you’re in a similar boat, don’t be afraid to experiment with different tools until you find what works best for your body.
A word of advice: when tracking longer cycles, you’re likely going to spend the majority of your time in a long follicular phase. Consistency is key when it comes to “catching” ovulation, so don’t give up if ovulation is delayed. Keep charting BBT and LH, so you don’t miss your ovulation signs!
Fertility awareness with PCOS can feel like a wild ride, but with the right tools and a bit of patience, you can find your rhythm. Remember, everyone’s body is different, and what works for one person might not work for another. So, give yourself grace, stay curious, and keep learning about your unique cycle.